
In Kenya, SMS text message reminders increased rates of clinic attendance on scheduled days compared to standard care. In another study, SMS text message reminders were utilized when patients were delayed in opening their medication bottles, and increased TB cure and smear conversion rates were reported compared to DOTS.

One example is a study in South Africa, where SMS text message reminders were equally effective compared to the more resource-requiring directly observed therapy, short-course (DOTS) strategy. A systematic review by Nglazi and colleagues found only four studies that compared the outcomes of the SMS text message intervention group with controls for promoting adherence to TB treatment. In a study with participants from Cameroon and Kenya, text messaging was found to have a significant effect on adherence to ART. Daily text messaging was found to be a feasible and acceptable way to remind HIV-positive youth with poor adherence to ART to take their medications, and there was a significant increase in adherence rates, postintervention. In Brazil, SMS text messages were able to help Brazilian women living with HIV/AIDS to remain adherent to ART for a period of 4 months. A study in Kenya examined adherence and found that weekly text messaging enhanced ART adherence and improved suppression of viral load.

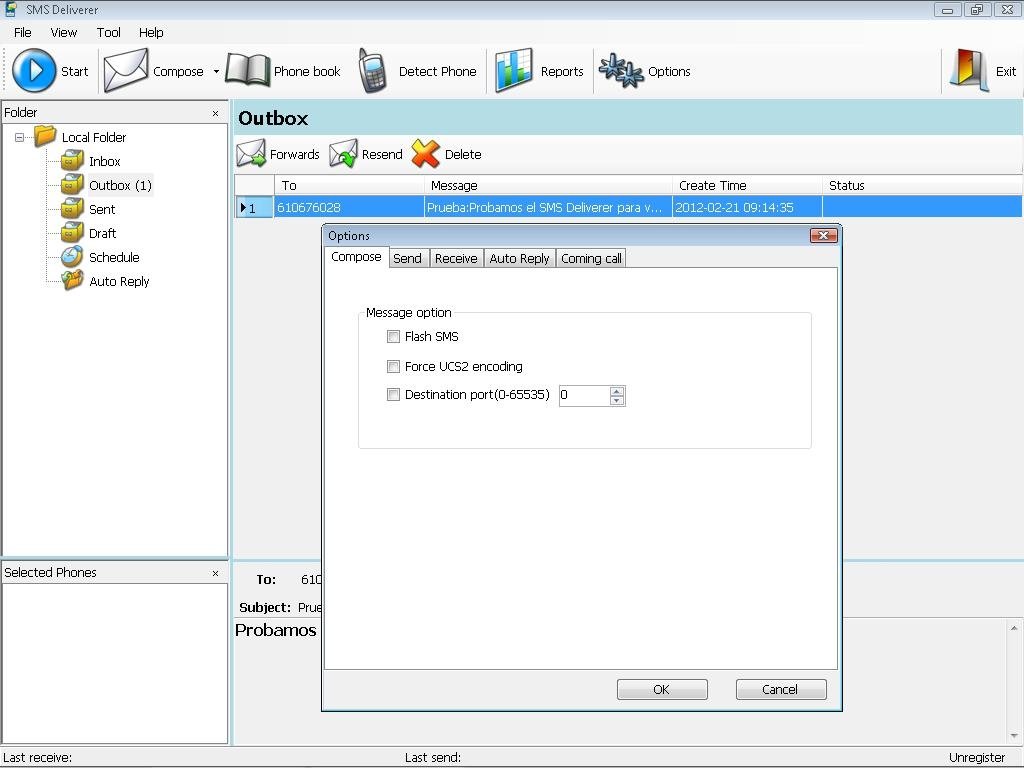
Įffects of the use of mobile phone text messaging on antiretroviral therapy (ART) adherence have been investigated in a number of studies. For example, mobile phones were incorporated into a central terminal for personal health examination, where a system referred to as mobile health examination launched on the phone (M-HELP) could generate electronic health records and send them to physicians via email or multimedia messages. This data could then be used to send medical recommendations to patients. For instance, mobile phones could be used to transmit data collected from a patient’s mobile phone to a remote system where data is processed and accessible for physicians. Mobile phones integrated with electronic health records (EMR)-in the context of HIV and TB programs called electronic patient tracking systems (EPTS)-could have the potential to empower the health care system and improve patients’ welfare, as well as help patients improve self-management of their disease. This may include operational decisions for short-term management of patient retention at individual care centers, tactical decisions such as reconfiguring the messaging based on performance, and strategic decisions such as data collection or preservation. But there is also a need for interactive program management by reacting promptly and effectively to deviations from program plans. Mobile phone short message service (SMS) text messaging is well suited for supporting self-management and improvement of patients' self-efficacy skills through, for instance, medication reminders and motivational text messages. It allows communication across geographic boundaries and reaches people directly where they are located. Due to the widespread use and low cost of this technology, it pervades all age groups and many cultures and socioeconomic backgrounds, including in developing countries. Mobile phone technology has the potential to serve as a strategic intervention medium to improve patient management.
While there may be many reasons for the lack of endurance, there may be ways to improve completion of treatment programs by maintaining better contact (communication) between doctors and patients. Hence, there is a need to improve the adherence and retention in care. One major problem with HIV/AIDS and TB treatment is ensuring patients pursue their treatment, including medication and medical checkups until completion. In 2013, nearly 140,000 developed TB and close to 18,000 died from the disease in Mozambique. In Mozambique, in 2012, 1.6 million were living with HIV and there were 120,000 new infections. In 2013, an estimated 9.0 million people developed TB and 1.5 million died from the disease, 360,000 of whom were HIV-positive. Of the global burden, Sub-Saharan Africa had 25 million people living with HIV and nearly 1.6 million new HIV infections. Globally, in 2012, an estimated 35.5 million people were living with HIV and some 2.3 million people were newly infected. HIV/AIDS and tuberculosis (TB) are major public health problems in many developing countries around the world.


 0 kommentar(er)
0 kommentar(er)
